
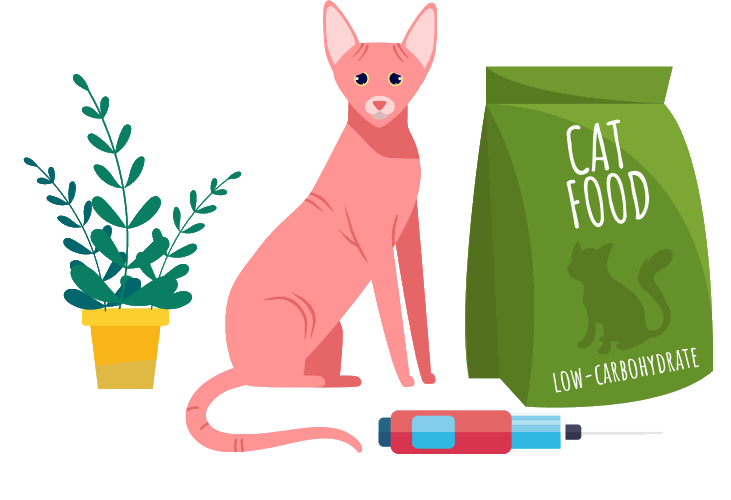
Diabetes, a hormonal condition which affects blood sugar levels, is well known in people. But did you know that cats can be diabetic too? In our feline companions, diabetes causes symptoms such as urinating and drinking more, as well as weight loss. More common in overweight, middle-aged to older cats, it is treated using insulin injections and a strict diet.
In this article, learn more about what diabetes is, the symptoms in cats, diagnosis, care and treatment.
Quick Overview: Feline Diabetes







What Is Diabetes?
Diabetes mellitus (usually just called diabetes) is a hormonal condition affecting sugar metabolism. It happens when there is not enough insulin in the body. This can be an ‘absolute deficiency’, where not enough insulin is made by the pancreas, or a ‘relative deficiency’ where there is insulin available but the body cannot respond to it (insulin resistance) – or a mixture of both!
Cats get a type of diabetes most similar to human Type 2 diabetics, where the body responds poorly to insulin, often combined with a lack of production.
Normally, each time your cat eats a meal, beta cells in their pancreas trigger the release of insulin, which streams into your cat’s blood and attaches to and unlocks cells, allowing them to absorb energy-giving sugar. Without insulin, glucose is incapable of converting to fat and energy in the body. If insulin is a key, glucose in a diabetic cat’s body is like a person locked out of their house. Unable to do anything useful, the sugar builds up in the blood.
Causes

Diabetes is more common in overweight and sedentary cats. Affected kitties are usually middle-aged or older.
Cats usually suffer from the Type 2 kind of diabetes, caused by abnormalities in their pancreas. Affected cats respond poorly to insulin, and also tend to have lower levels of insulin produced. Prolonged resistance to insulin, and high sugar levels, cause further damage to the pancreas, resulting in even less insulin being produced.
Diabetes can occur in any age or breed of cat, but tends to affect middle-aged and older cats. Some breeds, such as the Burmese, may have a genetic predisposition to develop diabetes, and so are at higher risk.
Risk Factors
As well as genetic factors, there are certain aspects of feline life that can make cats more prone to developing diabetes. Similarly to humans with Type 2 diabetes, the disease can be affected by dietary and lifestyle factors, and can be secondary to certain other conditions or medications.
Risk factors in cats include:
- Obesity
- A sedentary lifestyle
- Some medications such as steroids
- Some illnesses such as pancreatitis
Symptoms
The increased levels of sugar in the blood that are characteristic of diabetics lead to some common symptoms, as the cat’s body tries to flush the excess sugar out of its system. The signs can come on gradually over time, or appear quite suddenly.
Here are the common signs:
- Increased thirst (polydipsia)
- Increased urination (polyuria)
- Increased appetite
- Weight loss
- Lethargy
There are also some lesser known symptoms of diabetes in cats:
- Vomiting
- Weakness or collapse
- Increased likelihood of infections such as urinary tract infections
Complications of Diabetes

Cats with diabetes can become very weak and lethargic if the by-products of fat and protein digestion (ketones) build up in their body
Insulin is a really vital hormone, and changes to either the levels of insulin or the body’s response to it can cause a range of problems.
Insulin is crucial to maintain suitable blood sugar levels, but it’s also needed for the transfer of sugar from the blood to the cells. If the body’s cells are not receiving sugar for energy, they start breaking down fats and proteins instead.
This process can result in by-products called ketones, which can make pets very ill. A buildup of ketones in the body causes a condition called diabetic ketoacidosis (DKA). Signs that your cat is in a state of DKA include fruity or acetone-scented breath, lethargy, loss of appetite, vomiting and collapse.
A further complication is known as diabetic neuropathy. It affects about 10% of cats diagnosed with diabetes and usually develops after a few months of untreated diabetes. Diabetic neuropathy typically affects the femoral nerve (a major nerve in the leg), causing weakness of the legs and something called a plantigrade gait.
You and I have a plantigrade gait—we walk on the soles of our feet. Cats usually walk on their toes. When they have diabetic neuropathy, cats often walk on their hocks or heels. Diabetic neuropathy is usually reversible with glycemic control through insulin therapy, diet, and healthy lifestyle.
Diagnosing Diabetes in Cats
If your pet is showing any potential symptoms of diabetes, such as excessive thirst or urination, a trip to the veterinarian is recommended.
Your cat will need bloodwork and urine testing to diagnose diabetes, although it may be suspected after a physical examination and a discussion of the symptoms. The bloodwork and urine testing will reveal persistent high levels of glucose.
Stress in cats can cause them to have a transient rise in blood glucose, so your vet may need to keep your cat in the veterinary hospital for some further testing to ensure they definitely have diabetes. Your cat may also need to be hospitalized for stabilization and initial treatment.
Treatment
Diabetic patients usually require injections of insulin, once or twice daily. There are different types of insulin, and different methods of injection, so you and your veterinarian can discuss a treatment plan that works for you and your cat. Injections are usually given just after a meal, to reflect natural insulin releases which occur when eating.
Your pet will start on a fairly low dose of insulin, calculated based on weight and designed to prevent accidental hypoglycemia (low blood sugar). This dose will then need to be adjusted over the first few weeks, based on blood sugar measurements.
These measurements may be taken at the clinic, or some owners are happy to learn how to check their cat’s sugar levels at home, to reduce the stress of veterinary visits. It can take some time to stablize a diabetic, so be patient.
There are oral hypoglycemic medications available, to avoid having to inject. However, these drugs have a 5-30% success rate, which isn’t particularly impressive. Remember, insulin injection isn’t just more effective than pills – it’s safer.
In addition to potential hypoglycemia, oral diabetic drugs such as glipizide are associated with side effects including vomiting, loss of appetite, and jaundice. And as most people realize after a couple of weeks of trying to pill their diabetic cat twice a day, the reality of pilling a cat is more frightening than injecting your cat with a thin hypodermic needle!
As diabetes in cats is highly linked to factors such as obesity, diet and lifestyle, getting your cat onto the correct diet for a diabetic is really important. In some cases, diabetic cats can even achieve remission and stop requiring insulin injections! Your vet will be able to advise you, but it is generally recommended for diabetic cats to be on a high-fiber, low-carbohydrate food.
It’s easy to panic if your cat is diagnosed with diabetes. There’s no doubt that this is a serious disease, and requires fairly intensive management and ongoing care. Some owners may even consider that euthanasia may be the best option.
However, diabetes is very manageable in cats, and most respond very well to insulin and dietary change. The prognosis for a stable diabetic is very good, and although daily injections may seem daunting, both cat and owner usually adjust very quickly to the new routine.
How to Care For Your Diabetic Cat
A strict routine, and careful control of diet and insulin therapy are essential for diabetics
Diabetic patients require careful management to achieve successful control of their blood sugar. There are a few tips to consider at home.
Routine
Diabetics do best with a fairly strict schedule. Insulin injections and meals need to be given at set times of day for best effect, and diabetic cats shouldn’t miss a dose, or a meal. Appropriate weight management, controlled feeding and exercise schedules are all helpful for best management of this condition.
Watch Out for Signs
Diabetic cats need to be monitored carefully, as insulin requirements can change with age and progression of the disease. Cat owners need to pay attention to their cat’s litter box habits, appetite, thirst and weight.
Hypoglycemic episodes can also be a problem, so keeping an eye out for your cat being lethargic or wobbly is essential.
Keep Records
It can be really helpful to keep a diary if you have a diabetic cat. Record their insulin dose and their feeding schedule, and any changes to their routine. If you elect to monitor blood sugar levels at home, these need to be written down as well.
It can also be really useful to keep track of your cat’s thirst, appetite and weight. All of this information can help your veterinarian provide the best advice for your individual kitty.
Frequently Asked Questions
How can you tell if your cat has diabetes?
Diabetic cats are usually extremely thirsty, urinate a lot and lose weight despite a good appetite. They may also be sick, be prone to infections and be lethargic. Your vet can diagnose diabetes in cats with some blood tests.
How long can a cat live with feline diabetes?
Diabetes is usually diagnosed in middle-aged to older cats. If the cat is treated and the diabetes is stabilized, the prognosis is good and cats can live for years after diagnosis.
Do diabetic cats need a special food?
Cats with diabetes are usually recommended to be on a low-carbohydrate diet, with good levels of fiber and protein. There are specialized veterinary diets available, but also commercial foods will fit these requirements. Diet is important for diabetics, so discuss what would be suitable with your veterinarian.
-
Jacquie S. Rand and others, Canine and Feline Diabetes Mellitus: Nature or Nurture?, The Journal of Nutrition, Volume 134, Issue 8, August 2004, Pages 2072S–2080S, https://doi.org/10.1093/jn/134.8.2072S
-
Susan Gottlieb & Jacquie Rand (2018) Managing feline diabetes: current perspectives, Veterinary Medicine: Research and Reports, 9:, 33-42, DOI: 10.2147/VMRR.S125619
-
Jacquie Rand, BSAVA Manual of Canine and Feline Endocrinology, Chapter 13, pp 133 - 147, 2012 British Small Animal Veterinary Association








I WANT TO KNOW THE BEST, NOST EFFECTIVE WAY TO TREAT DIABETIC NEUROPATHY – STOP THE DETERIORIZATION IN MY CAT.